Over the last two centuries, developments in healthcare technology have completely changed the way we live our lives.
From the creation of the seemingly humble stethoscope to the precise delivery of proton beam therapy in cancer treatment – each invention has reduced pain and suffering, and improved the quality and longevity of human life.
1816 –Amplifying internal noise with the stethoscope
Prior to the early 1800s, if a doctor needed to listen to someone’s heartbeat, the only way to do so was by placing their ear to the chest of the patient. For women, this was an embarrassing experience, and so to try and resolve the issue, French physician Rene Theophile Laennec started using a wooden tube to amplify the internal noises.
The stethoscope is now so frequently used it has become synonymous with the healthcare profession. Indeed, research published in the Journal of Medical Internet Research in 2012 by Professor Moyez Jiwa claimed the stethoscope had the highest positive impact on the perceived trustworthiness of the practitioner seen with it than any other tool.
1895 – Seeing into the body via the X-ray
Wilhelm Conrad Röntgen won the first ever Nobel Prize for the invention of the X-ray in 1895, which he discovered by accident when experimenting with a Cathode Ray tube in his laboratory. He identified that x-rays produced by the Cathode Ray tube were electromagnetic energy waves that cannot penetrate high-density materials, such as bone and lead. Thanks to Röntgen, medics could now see inside their patient’s bodies for the first time without having to open them up.
One of the first manufacturers of x-ray tubes was Philips, which began making them in 1919. Over the course of the century, Philips has made continual improvements to x-ray equipment, such as adding the C-arm in 1955 enabling x-ray systems to change direction, developing a system to improve visibility of blood vessels in 1982, through to 2012 when it introduced a new technology that produces razor-sharp images while limiting the patient and doctor exposure to radiation.
1932 – Stimulating the heart with the pacemaker
The Pacemaker uses an electrical charge to stimulate a regular heartbeat. The very first of these devices was built in 1932 but was only tested on animals – possibly because the hand-cranked motor that powered could not be relied upon.
The technology developed and by 1958 the first pacemaker ever implanted in a human was given to Arne Larsson in Sweden. Sadly, this first device failed after only three hours.
The invention of long-life lithium batteries in the 70s helped the technology to really take shape, and about three million people worldwide now have one fitted. A wireless pacemaker is the latest iteration to be trialed. Whereas conventional pacemakers stimulate the heart tissue via electrical leads that are fed into the heart through a vein, this new version features a small receiver planted inside the heart, which receives acoustic waves that are converted into electricity.
1953 – The discovery of DNA
In 1953 when Francis Crick, James Watson, Maurice Wilkins and Rosalind Franklin discovered DNA and its double helix shape, little did the world know that our understanding of life was to be changed forever. Sixty years on, DNA technological applications remains one of the new frontiers in science with tremendous growth and discovery potential.
DNA is a code, a means of storing biological data, in the form of genes. It has given us insight into the lives of dead organisms, such as mammoths and Neanderthals; it has enabled the development of gene therapy and genetic engineering; and it is now being considered as a data storage device: in January, a team of Cambridge scientists encoded all Shakespeare’s sonnets, a video of Martin Luther King’s ‘I have a dream’ speech and Crick and Watson’s 1953 paper into DNA.
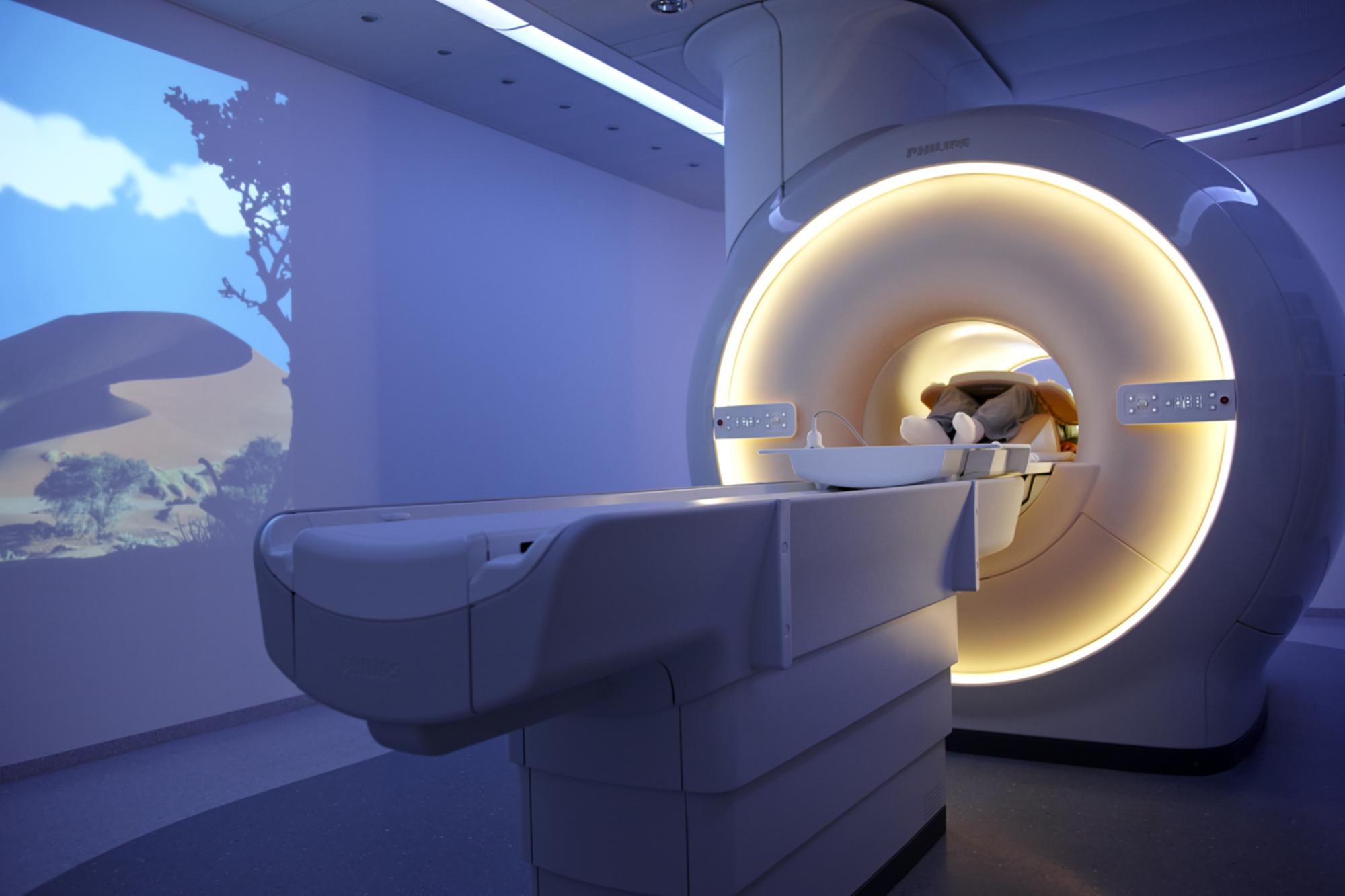
1977 – Revealing disease via the MRI scanner
In the 1970s, doctor and research scientist Raymond Damadian discovered that Nuclear Magnetic Resonance (NMR), which uses radio waves and magnetic fields to make atoms give off radio signals, could be used for medical diagnosis – cancer tissue, for example, emits a different response signal to healthy tissue.
On 3 July 1977, the first Magnetic Resonance Imaging (MRI) body exam was performed on a human being. It took almost five hours to produce one rudimentary image, and in the end Damadian’s technique was deemed impractical and never used.
Development of the technology continued, including by the healthcare technology company, Philips. Its latest MRI design, the Ingenia, is a revolutionary large aperture scanner, which uses 3D imaging, among other software, to enhance the visuals available to clinicians. Equally, it can be used in conjunction with Philips’ Ambient Experience solutions, which use sound and light to reduce anxiety and claustrophobia within the patient during the scan.
1989: Using high energy beams to treat cancer
Proton beam therapy uses a beam of protons to attack diseased tissue. The charged particles are directed at a particular area of the body where they damage the DNA of the cells, ultimately killing them or stopping their reproduction. It is primarily used in the treatment of cancer.
While treatments using energetic protons were used by scientists from 1946 onwards, it wasn’t until 1989 when the world’s first hospital based proton therapy centre was opened at the Clatterbridge Centre for Oncology in the UK. There are now 35 centres around the world, primarily in the US and Germany.
Delivering this therapy requires patients to spend considerable amounts of time in treatment centres. In America, Philips has been working with the IBA group to develop new centres and humanise this experience. For example, at the Willis-Knighton Cancer Center in Shreveport, Louisiana, Philips designers have used light, sound and images within the treatment room to help make the patient’s stay more comfortable.
2014: Delivering complex medical care remotely
Thanks to the internet, WiFi-enabled devices and cloud storage, patients no longer need to physically attend a hospital or doctors surgery to receive medical care and attention.
Take the Philips HealthSuite digital platform as an example. Using home-based and mobile devices, such as cuffs, patches, apps and other technologies, the HealthSuite allows the collection of patient vital signs, which are then sent remotely to a telehealth centre. This data is then quickly assessed and analysed – in real-time – by healthcare professionals, who can then implement the appropriate care package, be it increasing the amount of oxygen available to a patient with respiratory problems, or calling an ambulance for more serious matters.
Delivering healthcare in this way not only serves to maintain independence within the patient, but can help address some of the many challenges that health services face, such as increased demand for hospital beds and unnecessary emergency calls, thus reducing costs and enabling efficiencies.
This article is part of a thought-provoking series on living health, brought to you by the New Statesman in association with Philips, which looks at how technology, innovation and big data are helping to improve your health and our health-care system.






